🧵 View Thread
🧵 Thread (36 tweets)

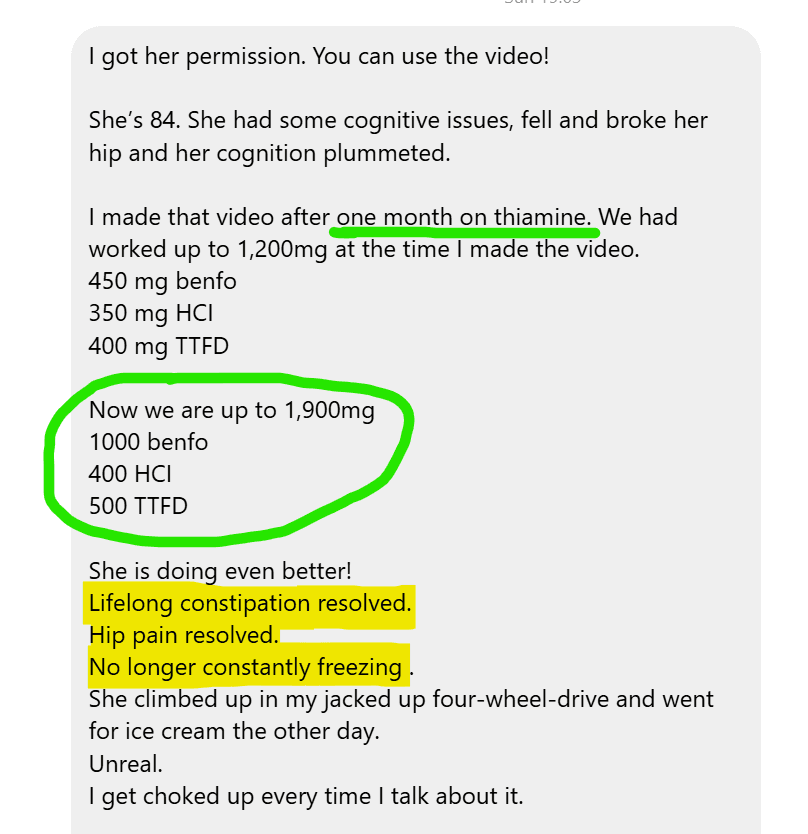
This what happens when you give mega-dose vitamin B1 to an 84 year old with Dementia 🧵 https://t.co/MbZAAIFkTo

She worked her up to 1,200mg total thiamine, using a combination of 3 forms - which provided good benefit However, after increasing the total dose to 1,900mg her mother saw even greater results: Lifelong constipation - gone Hip pain - gone Low body temp - gone https://t.co/8oWLgfnFIX

Using mega-dose B1 for dementia is not a novel concept There is a LOT of evidence showing impaired utilisation of B1 in the brain of dementia patients Many of the processes that drive dementia overlap with B1 deficiency https://t.co/NQwFQcGFIp

Such as faulty transport of vitamin B1 into the brain Or impaired utilisation by brain cells to generate energy https://t.co/lQgrR4VzE1

A "localized deficiency" of vitamin B1 in the brain has been suggested by experts in this field of research Meaning that many dementia patients would likely benefit from high doses of this nutrient https://t.co/xLN0JPylqA
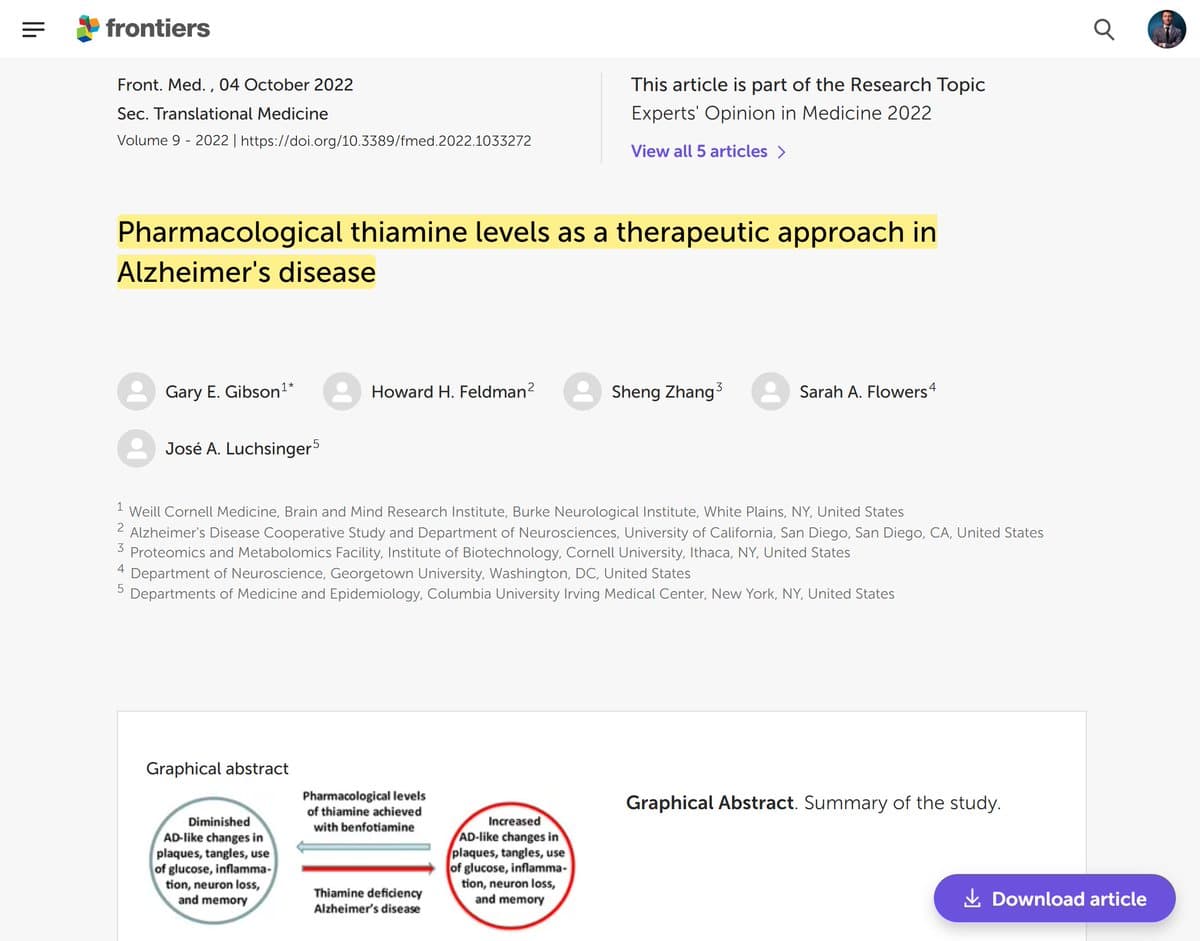

If you want to understand the nitty-gritty science, I discussed this concept in a lot more detail in the linked article below: "Keys to Neurodegeneration: Untapped potential for the aging brain? These mechanisms are particularly relevant in the field of neurodegeneration, where decades of research highlight a strong link between disrupted thiamine homeostasis and neurodegenerative processes. Notably, dysfunction of thiamine-dependent enzymes appears to be a hallmark feature of several neurodegenerative conditions, suggesting that localized thiamine dysfunction may be a key contributor to CNS vulnerability and disease progression. Alzheimer's Dementia (AD) A "localized deficiency" of thiamine in the brain has been proposed as a defining characteristic of AD (56), and is known to independently cause many of the key pathological changes including: impaired glucose metabolism (57), neuroinflammation (58), neuron loss (59), impaired cholinergic function (60) and greater presence of amyloid plaques and tangles (61). Disruptions of cerebral thiamine homeostasis and glucose metabolism have been identified (62), and activity of three thiamine-dependent enzymes are reduced in the brain (63,64). One of those is KGDH, whose activity is reduced by as much as 57% (65,66) which occurs in both genetic (67) and sporadic (68) forms of AD. Furthermore, Thiamine transporters decline (69) and metabolic impairments in the brain are closely related to TPP levels (70). Furthermore, levels of active TPP were significantly reduced in the frontal, temporal, parietal and occipital cortex in frontotemporal dementia (71) at autopsy. The synthetic thiamine derivative benfotiamine has been shown to counteract many of the pathological drivers of AD and cognitive decline (72), and a $45 milllon trial is currently underway in AD patients (73)." https://t.co/FXA9zspbsZ

Here's a basic overview of how to apply high-dose thiamine therapy: https://t.co/r4ZOOOFuZI

High Dose Thiamine Basic Guide: Principles & guidelines of this therapy What is thiamine? Thiamine (aka vitamin B1) is an essential water-soluble vitamin that plays a crucial role in how cells make energy. It is also very important for how nerves send messages throughout the body, and how the brain makes specific neurochemicals. It is found in a varierty of foods in low amounts: meats, organs, legumes, whole grains What does thiamine do? what does a deficiency look like? It is a key cofactor for enzymes involved in converting carbohydrates/fats/proteins into ATP, the body's primary energy source. Thiamine is especially needed for production of the neurotransmitter acetylcholine. It is therefore extremely important for the autonomic nervous system, and maintaining the balance between sympathetic and parasympathetic modes. From a conventional standpoint, a severe deficiency is known to affect the brain, heart, peripheral nerves, and gut. However, a mild deficiency can lead to a wide variety of NON SPECIFIC symptoms, which vary from person to person: Fatigue, brain fog, nerve pain, muscle pain, insomnia, anxiety, restlessness, autonomic nervous system problems/dysautonomia (blood pressure imbalances, vertigo, circulatio problems, heart rate problems, body temperature dysregulation), SIBO, stomach acidity imbalances, constipation, sometimes diahrrea, intestinal permeabilty and any number of function gut disorders. What causes a deficiency There are many potential causes. Thiamine status depends on carbohydrate intake, meaning the more carbs/sugar someone consumes, the greater demand for thiamine. -High intake of refined carbohydrate/refined foods - Alcohol destroys thiamine - Tannins (not caffeine) in tea/coffee inactivate thiamine - Medications: Metronidazole/flagyl, metformin, diuretics, omeprazole - Sulfites destroy thiamine - Chronic gut conditions which involve nutrient malabsorption/gut inflammation - Any state of prolonged physical stress (excessive exercise, critical illness, hyperthyroid, etc) In short, there are numerous things which can lead to/trigger a deficiency. A classical deficiency can be fairly straightforward to treat, but can take several months (depending on severity of the deficiency) However, there are also many individuals who don't display the risk factors, but respond to high-doses of thiamine. Here is where we will discuss the concept of "functional" or "localized" deficiency What is a “Functional” or "Localized" deficiency? This occurs in people who have normal systemic levels of thiamine in their body. However, certain regions of the body can experience a localized deficiency. For example, in neurodegenerative diseases, the research suggests localized "deficiency" in the brain. Without going into the mechanistic details, this can occur for various reasons, and can either be due to problems with transporting thiamine into the brain and into the cells. Or it can be related to problems with enzymes in cells which use thiamine. It can occur in the heart, the brain, the gut, etc. In this scenario, taking normal doses of thiamine is not enough. For people to see improvements in their condition, they generally require anywhere from 300-2000x the RDA (300mg to 2000mg, depending on the form of thiamine used) Here is where blood testing/functional testing becomes useless, because it doesn't measure what is going on at the organ/cell level of the affected area. Are tests useful? In general, no. They reflect recent intake for the most part. Even specialized tests like eTKA does not reflect what is occuring at the organ-tissue level (see above paragraph) Basic thiamine protocol Simple principles to follow: - Pick a form of thiamine - A B complex - A form of magnesium - An electrolyte supplement or additional potassium (either in supplement, or as coconut water) Different forms of thiamine: Thiamine HCL/mononitrate - Cheap but not well absorbed. Can be useful in high doses above 500mg Benfotiamine - well absorbed and gets into brain, good for peripheral neuropathy, diabetes, body pain, fatigue, alzheimers. Usually dosed between 150-2100mg TTFD (thiamine tetrahydrofurfuryl disulfide) - well absorbed and gets into brain - best for gut issues of any kind, POTS/dysautonomia and mood issues. Also good for fatigue, and neuropathy. Contains sulfur, so can trigger unwanted symptoms in some people. Molybdenum often helps this. Usually dosed between 100-500mg Basic Protocol - Start low and go slow with whichever form of B1 (think 10-50mg). Take B complex, magnesium and potassium source. - Gradually increase dose of thiamine over the space of days/weeks. - Watch for changes in symptoms. As increasing the dose, symptoms can get temporarily worse (called the paradoxical effect). If symptoms worsen, stay at current dose until they return to baseline. - When symptoms return to baseline, work on increasing dose again. Which brands to use? It doesn't actually matter which brand you use. I formulate supplements specifically for the purpose of "high dose thiamine" protocols, which are sold by my company Objective Nutrients - https://t.co/uUoxHlg6Rh However, I repeat: you can use whichever brand as long it contains what is stated on the label key points Sometimes people can take weeks/months to reach a dose that provides resolution in symptoms. Have patience. Thiamine is non-toxic. However, people often have a form which suits them best, and this should be experimented with. Each form does something slightly different. Mixing forms can be beneficial. This therapy likely only works in a MINORITY of people, although we don't know the exact number. If trialled for a few months and no change, it might not be for you. That's OK - it was worth a try! This is a BASIC guide and is a super condensed/simplified version of the full protocols in the proper guide. However, for most, it should work. That said, for people with complex health conditions, they often need to juggle some other things. Diet, other supplements, other therapies etc. There is complexity, and way beyond the scope of this introductory post. For that, i would recommend my PDF guide here: Thiamine Deficiency Protocols & Addressing Nutrient Interactions - https://t.co/nUdlGtdQeF Conclusion Hopefully this post provides you with enough information to get started. It should not be overly complex, and is quite simple for the majority of people

@mmilanovic Thiamega contains 400mg combined of 4 different forms, 3 of which were used in this lady https://t.co/y6sKcPuWOH Will be restocked in about a week

@BioavailableNd @EO_Nutrition I believe it!https://t.co/DvTXPZqGOk

@EO_Nutrition The B1 has knock on impacts on gut health as well, so it can def improve things. Focusing on gut health should help augment it."Dietary Vitamin B1 Intake Influences Gut Microbial Community and the Consequent Production of Short-Chain Fatty Acids"https://t.co/nsxF8iN5yY

@EO_Nutrition B1 helping gut health may also explain findings around improved liver health. There is currently a trial exploing using FMTs to fix liver cirrosis/ suspected mechanism of action is Butyrate.Thiamine/B1 seems to be improving gut to make SCFAs better.https://t.co/wpEdUKZrV5

@kitten_beloved @sonikudzu @Scaevolus @seconds_0 Maybe we could understand root cause for Thiamine going low & fix it across this constellation fo disorders."underscore the need for prompt, effective thiamine supplementation in all patients with chronic liver failure." [2008]https://t.co/M0yhUo8Z2Lhttps://t.co/MMUHP1kE7T

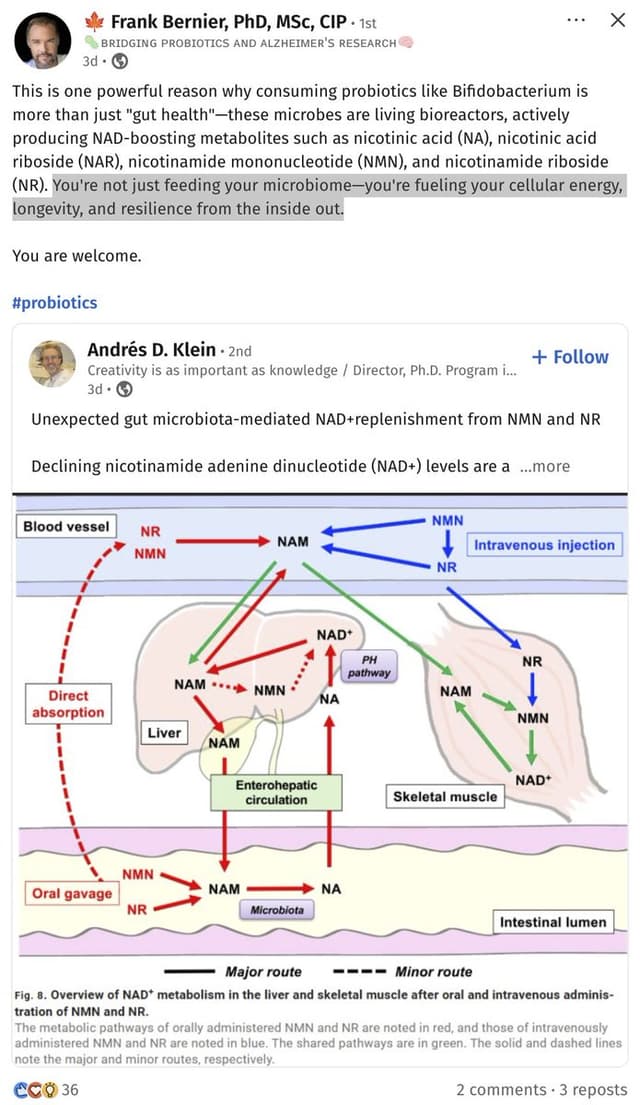
@EO_Nutrition When you see that one of the main things B1 does is act on gut health, and that gut bacteria themselves can make B1, it explains a lot of seemingly unrelated findings.https://t.co/W5SVu0hjU2

@EO_Nutrition You can then start using auxiliary therapies to help augment and restore the gut function and make the B1 supplementation work even better.https://t.co/jtf8kiNXan

@DavidPerlmutter Reduce the risk of Alzheimer's by promoting gut health.> "In conclusion, we show that kefir in natura, as well as its fractions may be promising therapeutic source against AD, modulating amyloidogenic related pathways."https://t.co/pLbIKrmoGEhttps://t.co/VcyTCVYAYi

@EO_Nutrition The weirdest thing I Found is that while B1 levels in teh blood stay fairly stable, the levels of B1 excreted into the gut can still be low. If you take a megadose of B1, once the body researches saturation it will give the rest to our gut frens.https://t.co/hSVEqXcE35

@EO_Nutrition My own constipation started going away once I realized that B1 problems tied to Crohn's could be partly mitigated by avoiding "anti-nutrients" from plants. Keto helped me there. Putting B1 back in also made the problems less intense.

@EO_Nutrition Had luck with external fermentation and heavily controlled diet, but didn't get remission until an FMT.Now my body doesn't have problems digesting plants. Gut seems to compensate for anti-nutrients if you let it. Feeding missing nutrients is a key insight to accelerate this.

@ultimape Reading your posts, it looks like we connected many of the same dots. It reference all of the studies you mentioned: Here is the abstract https://t.co/NSJqCNpDys

@EO_Nutrition Ah fantastic. Did you see Akkermansia muciniphila is able to support niacin + choline production? That may be one of the bigger ones improved gut health ala B1 ends up supporting. It showed up in a year on it's own after my FMT. Helps Nicotinic acetylcholine receptor activity.

@EO_Nutrition There's secondary things this may be impact on in particular around colonocyte health. Butyrate and Niacin seem to be key to functional NAD+ health.https://t.co/ZjMzVoOD5J

@EO_Nutrition This may explain why: https://t.co/kT2rmW9YBC

@EO_Nutrition Would appreciate your recommendation for someone who has been diagnosed with Parkinson’s. He took 100 mg. of sublingual B1 tablets and then tried 100 mg. Thiamix capsules without getting any relief or help from tremors. His lab results B1 = 194 (normal range is 70-180 nmol/L)